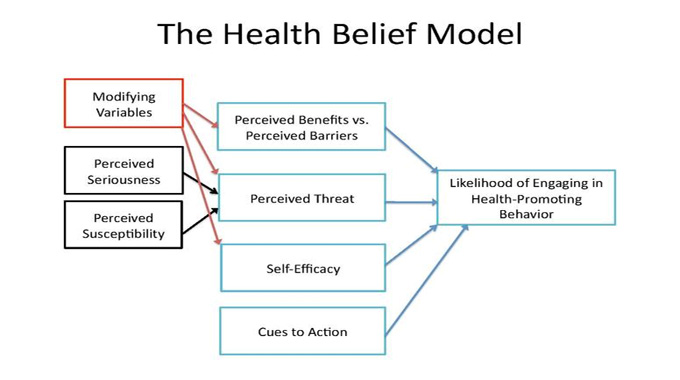
The Health Belief Model explains why patient patients can either accept or rejecting various health-related therapies or adopt appropriate healthy behaviors. The Health Belief Model predicts that individuals will react best to messages regarding disease prevention or health promotion if the following four criteria for transformation exist:
An Array of Potential Diseases, Illnesses, and Situations
The individual recognizes the threat to his health presented by an array of potential diseases, illnesses, and situations. An individual who fears he or she will become ill, is overweight, or has poor health will likely refuse to take any health-related action. Likewise, a fearful individual who lacks motivation to engage in physical activity will not use a walking stick, watch, bike, or participate in any other health action. In addition, an idle individual lacking motivation to work out will not eat healthy foods, won’t get regular exercise, or engage in any other health activity. Similarly, an individual who lacks motivation to make positive lifestyle changes will fail to make any health improvement.
The Health Messages
The health belief model also predicts that there will be little or no correlation between health behaviors and self-efficacy for acceptance of health messages. The absence of internal and external cues will only lead to partial or complete rejection of health messages. External cues such as reminders, motivators, and motivating words will only lead to partial or complete success in changing behaviors or attitudinal cues. For example, if a patient’s physician prescribes diet restrictions, she may feel compelled to obey these restrictions if she believes that she lacks the self-efficacy to control her own eating habits. However, if a similar condition is absent, she will not be motivated to adopt healthier behaviors or change her dietary habits.
The Health Behaviors
The health belief model also predicts that interventions designed to change health behaviors will have minimal impact when health beliefs are intact. However, these interventions may have increased the perceived barriers to behavior change. This is because many people perceive health interventions as intrusive and costly. When there are clear health interventions, they are more likely to be adopted. However, if an intervention requires a person to admit he or she has a problem, the behavior may not change. Because the perceived barrier to change is the same, both interventions will have minimal impact.
The Health Interventions Necessary
The health belief model also predicts that the presence of multiple cues will likely increase the number of health interventions necessary to bring about change. For example, if a person feels she faces at least three significant barriers to behavior change, she will be likely to require at least four interventions to bring about a significant change in her health. Similarly, if she faces at least three major barriers to health improvement, she will be likely to need at least four interventions to bring about a major change in her health. Each additional barrier that a person faces decreases the number of interventions necessary to bring about a change in her health. This means that the presence of one barrier lowers the perceived threat of behavioral change and increases the likelihood of behavioral change.
Outline
It is important to note that the health belief model (HBM) is not intended to replace the patient’s own judgment in assessing her health-related status. It should be remembered, however, that the model can be instrumental in improving a person’s awareness of her health-related status and in identifying those gaps in her life that may hinder her from achieving desired health outcomes. In this way, it can help to ensure that individuals who are at risk for health problems are made aware of the potential benefits of preventive care, treatment, and behavioral interventions that can transform their lives for the better.